Pediatric Airway Atlas
Infants and children with abnormalities of the upper airway are at risk for hypoxia, respiratory insufficiency and long-term morbidity. Multiple concurrent levels of upper airway obstruction frequently occur, leading to difficulties in air exchange, coordination of swallow and speech development. In children with these conditions, a multidisciplinary approach to care involves selection from a variety of potential medical and surgical interventions. In these unique and challenging cases, therapy is typically directed by the clinician’s experience and preference, rather than on normalized physiologic or anatomic metrics. In some cases, initial treatment failures occur leading to potentially serious complications and the need for invasive procedures.
As computer technology has become more advanced, powerful bioengineering tools are now available for investigating physiological dynamics in the respiratory tract. Three-dimensional computational models can be generated from patient-specific digital data captured by computed tomography (CT) scans. Computational fluid dynamics (CFD) and fluid-structure interaction models compute airflow, wall shear stress, pressure distribution, and (most recently) self-consistent treatment of airway wall shape change due to the airflow.
Furthermore, the computed geometry can be virtually modified to simulate medical intervention, surgical techniques, and normal growth and development. These computational models will enable “virtual surgery” and virtual “wait and watch” to estimate the effect of different interventions.
Our long term goals are to use a functional computational model as a novel, noninvasive clinical tool to evaluate the pediatric airway for diagnosis of airway anomalies; to model and predict the effect of therapies on airway patency and secondary functions such as speech and swallowing; and to guide medical and surgical management of upper airway obstructive lesions in pediatric patients.
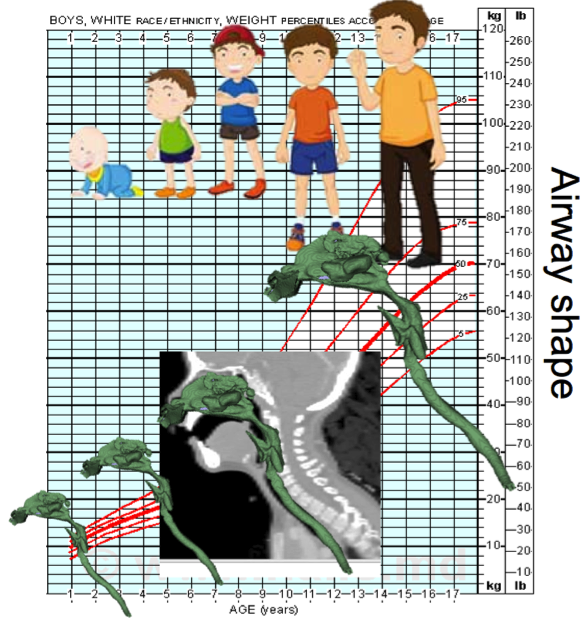
Our image analysis work so far has focused on developing method to develop a pediatric airway atlas [1] and associated methods for airway characterization [2]. The airway atlas is built from a normal control population and currently captures cross-sectional airway areas over time and expected airway variation. This allows us for an individual child to compute an age adapted airway atlas, which can be used to assess how the child’s airway compares to what is typically seen at the child’s age. This is conceptually similar to a standard growth chart, but operates on full descriptions of airway cross sectional areas.
References:
[1] Y. Hong, M. Niethammer, J. Andruejol, J. Kimbel, E. Pitkin, R. Superfine, S. Davis, C. Zdanski, B. Davis, “A Pediatric Airway Atlas and Its Application in Subglottic Stenosis.” ISBI 2013.
[2] Y. Hong, B. Davis, J. Marron, R. Kwitt and M. Niethammer, “Weighted Functional Boxplot with Application to Statistical Atlas Construction,” accepted to MICCAI 2013.