Lung Cluster
The lung is the site of gas exchange with the bloodstream, and maintaining the necessarily large surface area of a gas/liquid interface free of pathogens is a truly remarkable feat. From the first breath, tissue layers in contact become separated to allow the inflow of gas. Without a molecular layer of surfactant, this separation is impossible. Once gas flow into the lung is established and maintained in the newborn, the next challenge emerges. Each hour the lung inhales millions of pathogens that must be cleared before infection ensues. This is achieved through the trapping of the pathogens in a viscoelastic layer of mucus, and the subsequent flow of mucus, through air and ciliary propulsion, out of the lung. The failure of this clearance mechanism is fatal. CISMM supports three projects within the Lung Cluster studying these phenomena.
The Virtual Lung Project is creating an integrated model of mucus clearance.
Biophysical Properties of Mucus is studying the polymer physics and biology of mucus.
Lung Surfactant Rheology is developing tools for measuring the rheology of molecular monolayers.
Microfluidic and Biomimetic Cilia Systems are providing new insights into biological cilia and fluid flow.
Pediatric Airways simulates the impact of various surgical interventions on children with upper-airway disorders.
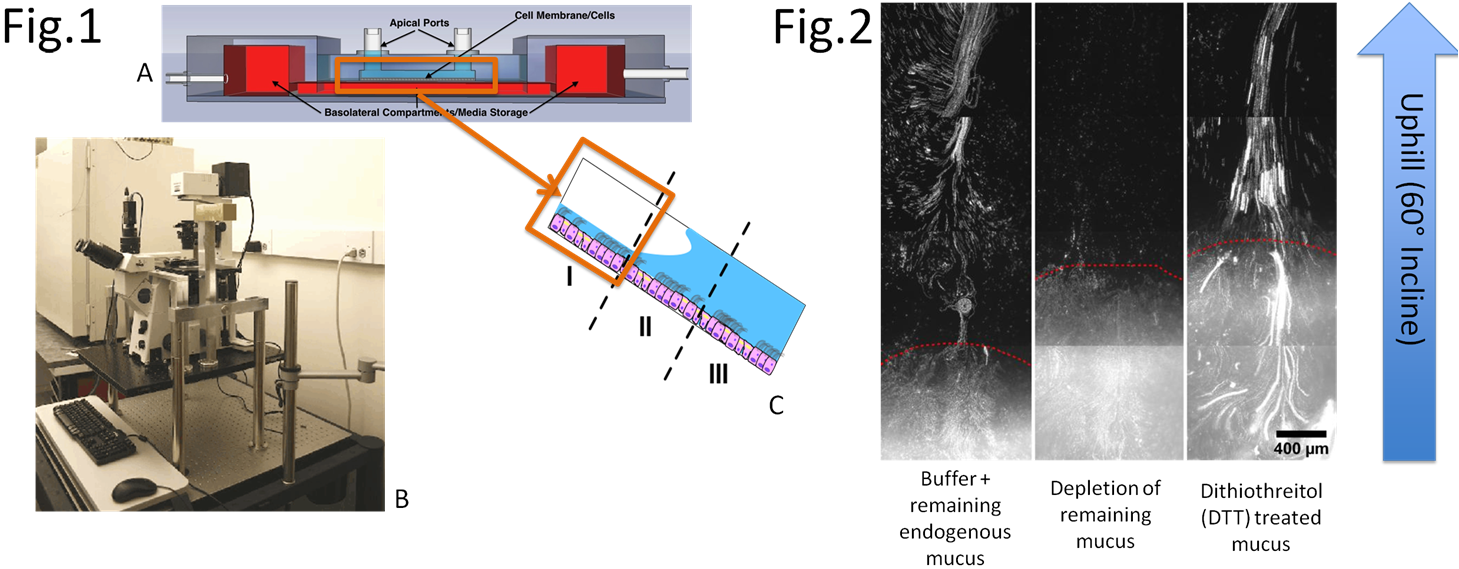
Mucociliary Clearance Assay
Mucociliary clearance (MCC) is vital for the maintenance of human lung health and function, and many airway diseases are related to MCC dysfunction, such as Cystic Fibrosis (CF) and Chronic Obstructive Pulmonary Disease (COPD). Understanding and treating failed clearance in the disease state will be aided by a complete understanding of the mechanism of healthy, successful MCC. We present a novel cell culture bioreactor and imaging system that allows us to study clearance against gravity. We’ve shown that liquids that transport horizontally don’t necessarily transport against gravity, however, healthy mucus transports in both systems. Through the use of specifically chosen simulants (polymer gels) that share known rheological or biochemical characteristics with mucus, and comparing their clearance rates to those of healthy mucus, it is possible to span the parameter space and distinguish between rheological and biochemical characteristics of mucus and determine which are necessary and sufficient for successful MCC. This will help establish a model for healthy MCC, which can be compared to disease state MCC to understand the mechanism behind unsuccessful transport. These determinations could lead to targets for treatment of chronic pulmonary diseases.
Mucociliary Adhesion Assay
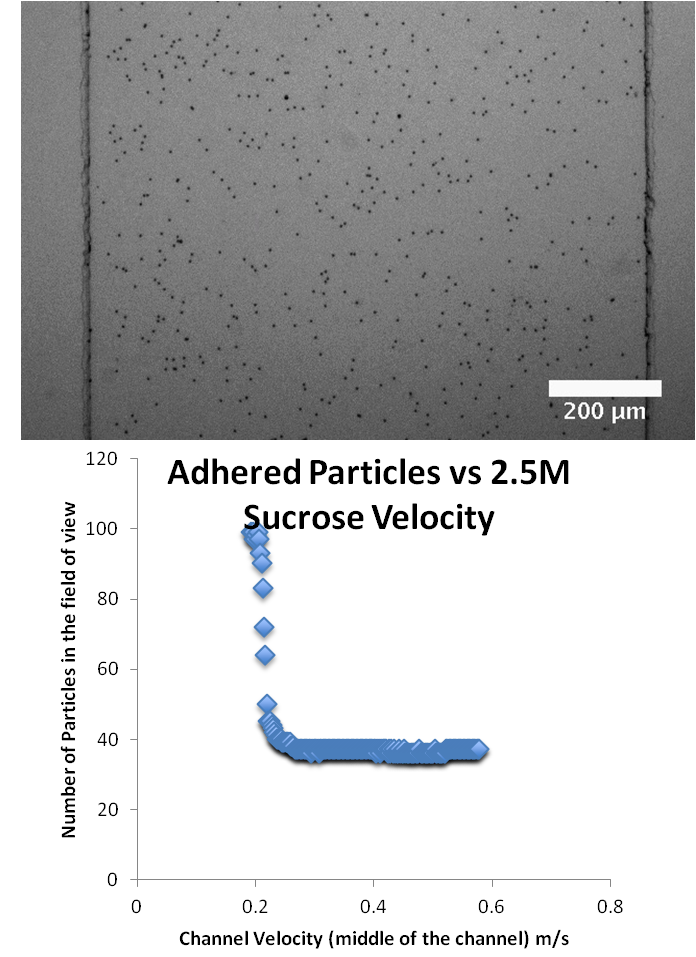 Mucociliary clearance is an essential part of airway health and sterility. Adhesion plays an essential role in the interaction between pathogens and mucus, and new evidence points to adhesion playing a key role in the interaction between mucus and cilia. To better understand and quantify these adhesion interactions, we are building and developing an adhesion assay to test these interactions. Specifically our adhesion assay employs a syringe pump to deliver a shear-stress to human bronchial epithelial cells grown in a microfluidics system. By using specifically functionalized beads we can use the system to identify specific binding interactions between the bead functionalization and the epithelial surface, which includes cilia, mucins, and the cell glycocalyx. In addition to identifying interactions, we can also use our system to quantify the strength of adhesion between the binding partners. Once we’ve identified these partners, we can then apply this to our clearance assay and explicitly look at the contribution that adhesion plays in clearance at a Vertical Air-Liquid Interface.
Mucociliary clearance is an essential part of airway health and sterility. Adhesion plays an essential role in the interaction between pathogens and mucus, and new evidence points to adhesion playing a key role in the interaction between mucus and cilia. To better understand and quantify these adhesion interactions, we are building and developing an adhesion assay to test these interactions. Specifically our adhesion assay employs a syringe pump to deliver a shear-stress to human bronchial epithelial cells grown in a microfluidics system. By using specifically functionalized beads we can use the system to identify specific binding interactions between the bead functionalization and the epithelial surface, which includes cilia, mucins, and the cell glycocalyx. In addition to identifying interactions, we can also use our system to quantify the strength of adhesion between the binding partners. Once we’ve identified these partners, we can then apply this to our clearance assay and explicitly look at the contribution that adhesion plays in clearance at a Vertical Air-Liquid Interface.